Osteoporosis is a common disease that causes a thinning and weakening of the bones. It can affect people of any age. Women have the greatest risk of developing the disease, although it also occurs in men. Osteoporosis affects 55% of Americans aged 50 or older; one-half of women and a quarter of men will fracture a bone as a result of low bone density (osteopenia) or osteoporosis. Thin bones are the cause of 1.5 million fractures per year in the United States; hip fractures alone result in 300,000 hospitalizations. It is important to diagnosis low bone density or osteoporosis early so that steps can be taken to rebuild bone strength and lessen the risk of fracture.
What is Osteoporosis?
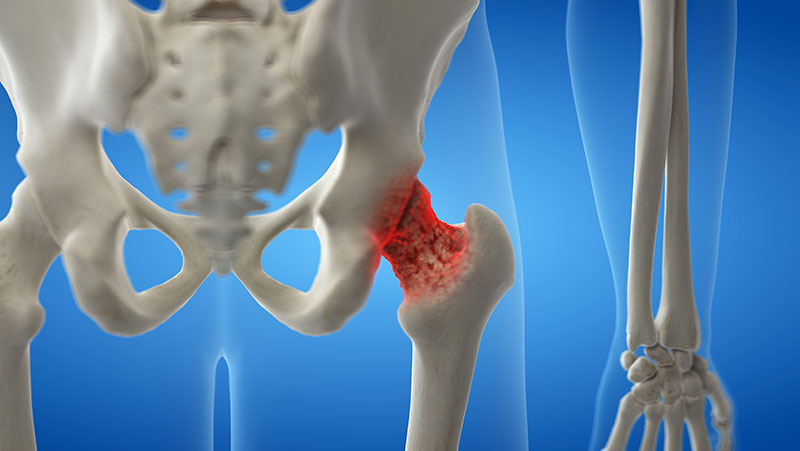
Osteoporosis is a bone disease characterized by low bone density (thickness of the bone), decreased bone strength, and a change in the bone structure, which can lead to an increased risk of fracture. The normal bone structure becomes thinned out and porous with poor nutrition, aging, or when osteoporosis develops, lessening the ability of the bone to withstand the typical forces that are applied in everyday living. Fractures from low bone density and osteoporosis can be serious, causing pain and affecting quality of life.
Bone is living tissue. Normally, one type of cell removes bone and another type of cell adds bone in a balanced, ongoing process. In osteoporosis, bones weaken when not enough new bone is formed and/or too much bone is lost. This imbalance commonly begins in women during the first 5 years of menopause. However, it can also occur in men and in children, often due to diseases that affect bone development, such as celiac disease, inflammatory bowel disease, rheumatoid arthritis, spina bifida, cystic fibrosis, or kidney disease. Some medicines, such as steroids, may increase the risk of developing osteoporosis. Athletes who are underweight during the time of peak bone development are also susceptible.
There are many factors that can cause a person to be at risk for developing osteoporosis. It is important to know your risks so that you can be diagnosed and proactive in your treatment.
Risk Factors for Osteoporosis
Noncontrollable risks
- Female gender
- Small frame
- Advanced age
- Hormone levels
- Genetics
- Predisposing medical conditions
Controllable risks
- Cigarette smoking
- Excessive alcohol intake
- Inactive lifestyle
- Excessive caffeine intake
- Lack of weight-bearing exercise
- Drugs (eg, steroids, heparin)
- Poor health
- Low weight
- Calcium-poor diet
- Low vitamin D levels
How Does It Feel?
Osteoporosis is a disease that can be “silent.” There may be no outward symptoms until a fracture occurs. If you are middle-aged or older, you may notice a loss of height or the appearance of a humpback. You may also begin to experience pain between your shoulder blades or above the crest of the pelvis.
People with low bone density may experience fractures in everyday situations that would not occur in persons with healthy bones, such as breaking a hip or a wrist with a fall from a standing height, breaking a rib when opening a window or when receiving a hug, or breaking an ankle after stepping off a curb. These are called fragility fractures and are a red flag for bone disease. Spinal compression fractures, particularly those in the upper back or thoracic spine (area between the neck and the lower back), are the most common fractures, followed by hip and wrist fractures.
How Is It Diagnosed?
If you are seeing a physical therapist for back pain or other rehabilitation issues, the therapist will review your medical, family, medication, exercise, dietary, and hormonal history, conduct a complete physical examination, and determine your risk factors for osteoporosis. The assessment may lead the physical therapist to recommend further testing.
Osteoporosis is best diagnosed through a quick and painless specialized X-ray called the DXA, which measures bone density. The results are reported using T-scores and Z-scores.
- The T-score compares your score to that of healthy 30-year-old adults. If you have a T-score of -1 or less, you have a greater risk of having a fracture.
- If the T-score is -2.5 or less you will receive the diagnosis of osteoporosis.
- The Z-score compares your bone mineral density to those of the same sex, weight, and age. It is used for those whose bone mass has not yet peaked, premenopausal women, and men older than 50.
Other methods of measuring bone density include X-ray, ultrasound, and CT scan.
How Can a Physical Therapist Help?
Your physical therapist can develop a specific program based on your individual needs to help improve your overall bone health, keep your bones healthy, and help you avoid fracture. Your physical therapist may teach you:
- Specific exercises to build bone or decrease the amount of bone loss
- Proper posture to protect your spine from fracture
- Proper alignment during activities of daily living
- How to improve your balance so as to reduce your risk of falling
- How to adjust your environment to protect your bone health
Healthy bone is built and maintained through a healthy lifestyle. Your physical therapist will teach you specific exercises to meet your particular needs.
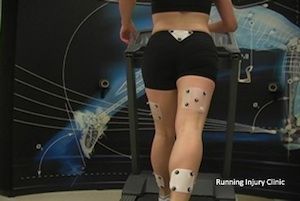
The exercise component for bone building or slowing bone loss is very specific and similar for all ages. Bone grows when it is sufficiently and properly stressed, just as muscle grows when challenged by more than usual weight. Two types of exercise are optimal for bone health: weight-bearing and resistance.
It is best for a physical therapist to provide your individual bone-building prescription to ensure that you are neither overexercising nor underexercising. Typically, exercises are performed 2 to 3 times a week as part of an overall fitness program.
Weight-bearing exercises
- Dancing
- Jogging (if your bone density is higher than -3.0)
- Racquet sports
- Heel drops
- Stomping
Resistance exercises
- Weight lifting in proper spine and lower-extremity alignment
- Use of exercise bands
- Gravity resistance (eg, push-ups, prone trunk extension with cushion to protect lowest ribs, single-leg heel raises, squats, lunges, sustained standing yoga poses in neutral spine position)
- Exercises that reduce or stabilize kyphosis (hunchback)
- Balance exercises
If you are diagnosed with osteoporosis or low bone density, your physical therapist will work with you to:
- Build bone or lessen the amount of bone loss at areas most vulnerable to fracture through exercise—hip, spine, shoulder, arms.
- Improve your dynamic balance to avoid falls.
- Improve your posture.
- Adjust your work and living environments to limit risk.
- Help you avoid exercises and movements that may contribute to spinal fracture, including any type of sit-up or crunch, and excessive spinal or hip twisting.
Conservative treatment of a fracture includes bed rest and appropriate pain treatment. Your physical therapist will work with you to:
- Decrease your pain through positioning and other pain-relieving modalities. Individualized physical therapist regimens can help reduce pain without the need for medications, such as opioids.
- Provide appropriate external devices, such as bracing, to promote healing and improve posture.
- Decrease your risk of a fall, strengthen your muscles, and improve your postural alignment.
- Avoid exercises that involve too much forward or side bending or twisting.
- Avoid water or endurance exercises, as they have been shown to negatively affect bone density.
If your pain lasts longer than 6 weeks following a spinal fracture, you can discuss surgical options, such as vertebroplasty or kyphoplasty, with your physical therapist, primary care physician, and surgeon.
Children and adolescents. Physical therapists can educate families and youth groups on proper exercise and posture, and about the need to move daily to build bone strength and prevent bone loss. Children with health issues such as spina bifida, diabetes, Crohn’s disease, and cerebral palsy are at a greater risk for bone disease and can particularly benefit from the guidance of a physical therapist. Proper physical conditioning is crucial for children and adolescents: the majority of bone is built during adolescence and peaks by the third decade of life.
Middle-aged and older adults. As people age, they may begin to notice postural, balance, and strength changes. Physical therapists work with middle-aged and older adults to:
- Develop individualized exercise programs to promote bone growth or lessen bone loss
- Improve dynamic balance to avoid falls
- Improve posture
- Improve the strength of back muscles
- Improve hip strength and mobility
Can This Injury or Condition Be Prevented?
Osteoporosis can be prevented by building adequate bone density through childhood, adolescence, and early adulthood. Building strong bones requires an adequate intake of calcium and vitamin D, and regular exercise.
There are steps to take to improve bone health at any age. An active lifestyle that includes resistance and weight-bearing exercise is important to maintain healthy bone. It is also important to avoid habits that promote bone loss, such as smoking, excessive alcohol consumption, and an inadequate intake of calcium in your diet. Maintaining good body mechanics and posture also contribute to good bone health. We have no control over the genetic tendencies we have inherited, but we can choose to manage osteoporosis through proper medication, diet, and appropriate exercise.
As with any health issue, an overall healthy lifestyle is important for staying well.
Real Life Experiences
Anna is a 69-year-old retired legal secretary. She has enjoyed her early years of retirement, taking long walks in beautiful settings across the United States. Two years into her retirement, however, she began having knee pain during some of her walks, which gradually grew worse. Last year, she had a total knee replacement due to arthritis. She now walks with a cane because of chronic knee and ankle pain, and has experienced a loss of balance. She also has developed a rounded upper back, and low back pain. She seeks the help of a physical therapist.
Anna’s physical therapist performs an assessment that includes a medical review for osteoporosis risk factors and for other health issues. He evaluates her range of motion and strength, testing her arms, legs, and trunk—especially her upper back. He tests the flexibility of her spine and her balance, her walking ability, and her risk of falling. Anna’s walking style is uneven and she leans heavily on her cane. A DXA scan reveals that Anna has lost bone density in her spine and both hips. A vertebral fracture assessment X-ray shows that she has painless compression fractures of her spine. Her physical therapist diagnoses osteoporosis of the spine.
Anna first works with her physical therapist to improve her posture and knee function through flexibility and strengthening exercises, so she can walk more normally while working on her balance to lower her fall risk. She tells him her main goal is to be able to take walks in the park again.
Anna’s physical therapist teaches her safe trunk movement to avoid spinal fracture. Anna agrees to wear a dynamic trunk brace 2 hours a day to help make her posture more upright. She practices weight-bearing exercises with considerations for her arthritis, and learns resistive strengthening exercises for her spine and hip. Anna’s physical therapist designs a gentle home-exercise program for her as well.
By her last visit, the flexibility and strength of Anna’s trunk and legs and her tolerance of physical activity have improved. The quality of her walking and dynamic balance are measurably improved, and her risk of falling has decreased. Anna feels much more confident about managing her condition.
Just this past week, Anna joined a therapeutic senior walking group that meets at the local botanic garden twice a week. She is thrilled to be enjoying gentle walks in nature again, and looks forward to coordinating other activities with her new group of friends!
This story was based on a real-life case. Your case may be different. Your physical therapist will tailor a treatment program to your specific case.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat those with osteoporosis. However, if you have a diagnosis of osteoporosis or low bone density, you may want to consider:
- A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in orthopedic physical therapy or geriatric physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
- A physical therapist who specializes in the treatment of osteoporosis.
You can find physical therapists with these and other credentials by using Find a PT, the online tool by the American Physical Therapy Association that can help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you’re looking for a physical therapist (or any other health care provider):
- Get recommendations from family and friends or from other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists’ experience in helping people who have osteoporosis.






:max_bytes(150000):strip_icc():format(webp)/a-man-stretching-his-hamstrings-in-the-gym-481713993-5717ba6a3df78c3fa232c519.jpg)
:max_bytes(150000):strip_icc():format(webp)/image-56cb3aeb5f9b5879cc542d6c.jpeg)
:max_bytes(150000):strip_icc():format(webp)/image-56ae1abd3df78cf772b98511.jpeg)
:max_bytes(150000):strip_icc():format(webp)/image-56a72ae53df78cf77292f366.jpg)
:max_bytes(150000):strip_icc():format(webp)/image-56a72add3df78cf77292f319.jpg)
:max_bytes(150000):strip_icc():format(webp)/image-565a831b5f9b5835e4679fb2.jpg)